An Atlas of Lumps and Bumps, Part 38: Lichen Striatus
Lichen Striatus
Lichen striatus is a benign, acquired, asymptomatic, self-limited T-cell mediated dermatosis.1-7 Also known as “Blaschko linear inflammatory papular eruption,” it is observed primarily in children.1-5
Lichen striatus is a relatively uncommon condition that typically affects children between 5 and 15 years of age.1-5,8,9 The condition is rarely seen in infants and adults.7,10 The female to male ratio is approximately 2:1.1-5 Lichen striatus has been reported in all ethnic groups with no known racial predilection.1-5 The condition is more common in the spring and summer.11 Approximately 60% to 85% of patients with lichen striatus have a personal or family history of atopic dermatitis, asthma, or allergic rhinitis.1-5
Lichen striatus usually occurs sporadically.1-4 Simultaneous familial occurrences have rarely been described.12-14 Hypersensitivity reactions, infection (e.g., varicella, influenza, human herpes viruses 6 and 7, group A β-hemolytic streptococcus, yeast), medications (e.g., etanercept, adalimumab, interferon, tumor necrosis-α inhibitors), vaccines (e.g., hepatitis B, Bacille Calmette-Guerin [BCG], measles, mumps and rubella [MMR], yellow fever), trauma, insect bite, vitiligo, and ultraviolet irradiation are possible predisposing factors.1-5,8,10,11,15-25 It is possible that a cross reactivity develops between the aforementioned antigens (e.g., vaccines, medications) and shared epitopes on keratinocytes which acts as a triggering factor.26
While the exact pathogenesis is not known, lichen striatus may result from environmental stimuli acting in a genetically predisposed individual.8,13,18 Many authors believe that lichen striatus is a form of cutaneous mosaicism in which an abnormal clone of keratinocytes arises due to a post-zygotic somatic mutation.11,27 In this situation, the body tolerates the aberrant clone until an acquired event such as a viral infection or trauma, which results in a T-cell mediated inflammatory reaction.27
Lichen striatus is characterized by a sudden onset of discrete, flesh-colored, tan, pink, or red, flat-topped lichenoid papules, usually 1 to 3 mm in diameter.7,14 Papules often coalesce to form a hyperpigmented continuous or interrupted linear band over a few weeks (Figure 1).1-5,14,28

Fig. 1. Lichen striatus is characterized by a sudden onset of discrete, flesh-colored, tan, pink, or red, flat-topped lichenoid papules that often coalesce to form a hyperpigmented continuous or interrupted linear band.
The linear band may develop a curved appearance as it follows Blaschko lines (the cutaneous lines of epidermal cell migration during embryonic development).1-5 The band may range from a few mm to 1 to 2 cm wide (most commonly 2 mm) and extends from a few cm to the full length of an extremity (Figure 2).8,28

Fig. 2. The band may range from a few mm to 1 to 2 cm wide (most commonly 2 mm) and extends from a few cm to the full length of an extremity.
Sometimes, two or more bands that parallel each other may be observed (Figure 3).1-5An S-shaped pattern on the anterior and lateral aspect of the trunk as well as a V-shaped pattern on the back are characteristic.19 In dark-skinned persons, the lesions may be hypopigmented (lichen striatus albus)1-5,18 Although lichen striatus may involve any part of the body, the arms and legs are most commonly affected.1-5,7 Typically, the lesion starts on a proximal extremity and extends distally.1-5 Other areas that may be involved include the trunk, buttocks, face, neck, and nails.19,29,30 Rarely, the rash is observed on the penis.7
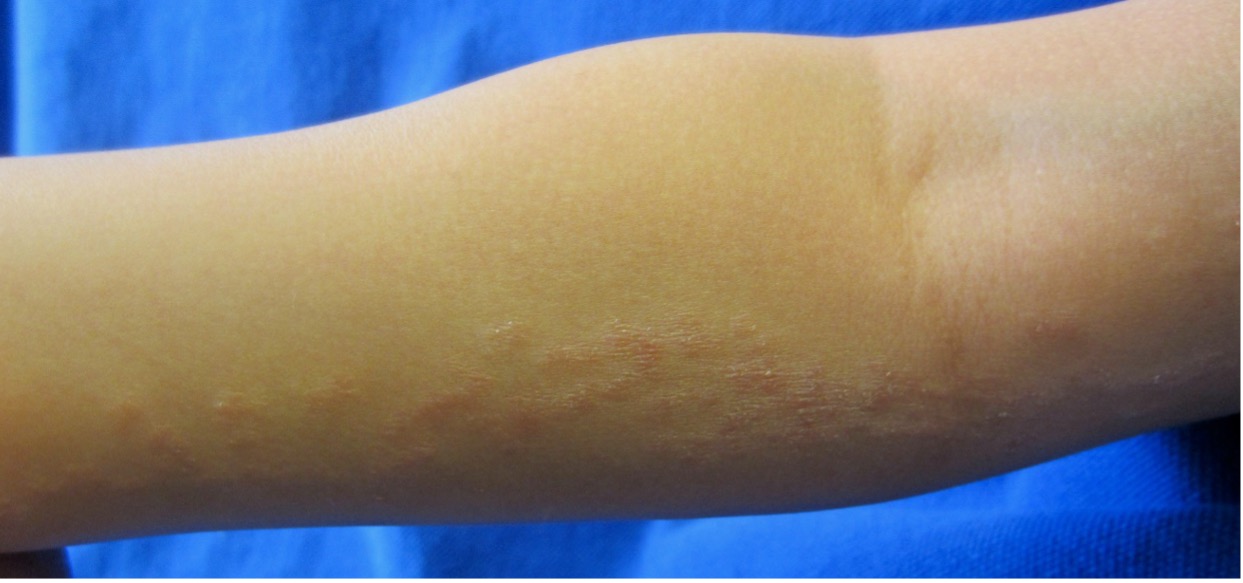
Fig. 3. A patient with multiple bands of lichen striatus is shown.
Typically, the rash is solitary and unilateral.28 V-shaped lines on the mid-back may be bilateral.1-5,19 Rarely, atypical forms with multiple and bilateral lesions have been described.18,31,32 The rash is usually asymptomatic.1-5,19 Pruritus is uncommon, except in those patients with atopy.1-5,10,19 However, when the onset occurs in adulthood, the lesions may be widespread and pruritic.33
>> Photoclinic: A Case of Adult-Onset Lichen Striatus by Milaan Shah, MD and Divya Shah, MD
Involvement of the nail is rare and is usually noted in association with typical skin lesions.6,19,34 However, nail involvement may occur before, after, or concurrent with the rash of lichen striatus.6,8,12,35,36 Very rarely, isolated lichen striatus can be limited to the nail unit without an associated cutaneous eruption.6,36 T-cell mediated inflammation of the nail matrix leading to defective keratin synthesis in the nail plate is believed to be responsible for the onychodystrophy.6,36 Nail changes may take the form of nail pitting, longitudinal ridging (onychorrhexis), splitting, fissuring, fraying, pitting, thinning of the nail plate, thickening of the nail plate (onychauxis), onycholysis, striate or punctate leukonychia, subungual hyperkeratosis, over-curvature of the nail plate, irregular transverse grooves, and, rarely, nail loss.6,12,19,34 Usually, only the lateral or medial portion of the nail plate of only one nail is affected,6,34,35 but polydactylous cases have also been reported.34
The diagnosis is usually made clinically based on the characteristic appearance of skin lesions and a pattern of distribution that follows the lines of Blaschko. Dermoscopic features include flesh-color (most common), red, white, brown, yellow lesion; gray granular pigmentations; erythematous blotches; white scar-like line; scales; and milia-like cysts.37 Further diagnostic work-up is usually not necessary. If the diagnosis is in doubt, a biopsy of the rash should be considered for histopathologic confirmation.
Lichen striatus can be cosmetically unsightly and can cause distress to patients. In addition, post-inflammatory hyperpigmentation and hypopigmentation may occur especially in dark-skinned individuals.8,12 The discoloration may last for months to years.8,12
Lichen striatus is a self-limited condition that often resolves within 1 year.13,28 Reverse Koebner response (resolution of the eruption with trauma) has rarely been reported.38 When associated with onychodystrophy, the rash tends to persist longer.9,34 Relapses may occur but are rare.1-5
AFFILIATIONS:
1Clinical Professor of Pediatrics, the University of Calgary, Calgary, Alberta, Canada
2Pediatric Consultant, the Alberta Children’s Hospital, Calgary, Alberta, Canada
3Dermatologist, Medical Director and Founder, the Toronto Dermatology Centre, Toronto, Ontario, Canada
4Associate Clinical Professor of Pediatrics, Dermatology and Skin Sciences, the University of British Columbia, Vancouver, British Columbia, Canada.
5Pediatric Dermatologist, the Pediatric Institute, Kuala Lumpur General Hospital, Kuala Lumpur, Malaysia
CITATION:
Leung AKC, Barankin B, Lam JM, Leong KF. An atlas of lumps and bumps, part 38: lichen striatus. Consultant. 2024;64(4):e3. doi:10.25270/con.2024.04.000002
CORRESPONDENCE:
Alexander K. C. Leung, MD, #200, 233 16th Ave NW, Calgary, AB T2M 0H5, Canada (aleung@ucalgary.ca)
EDITOR’S NOTE:
This article is part of a series describing and differentiating dermatologic lumps and bumps. To access previously published articles in the series, visit: https://www.consultant360.com/resource-center/atlas-lumps-and-bumps.
REFERENCES
1. Leung AKC, Kao CP. Keratosis pilaris. Consultant for Pediatricians. 2004;3:188-191.
2. Leung AKC, Robson WL. Lichen striatus. In: Lang F, ed. The Encyclopedia of Molecular Mechanisms of Disease. Berlin: Springer-Verlag, 2009;1170-1171.
3. Leung AKC. Lichen striatus. In: Leung AKC, ed. Common Problems in Ambulatory Pediatrics: Specific Clinical Problems, Volume 2. New York: Nova Science Publishers, Inc., 2011;267-270.
4. Leung AKC, Barankin B. Lichen striatus. Clin Case Rep Rev. 2015;1(1):1-3. doi: 10.15761/CCRR.1000101
5. Leung AKC, Barankin B. A linear band of erythematous, flat-topped papules on the forearm: Lichen striatus. Paediatr Child Health. 2018;23(4):260-261. doi: 10.1093/pch/pxy009.
6. Leung AKC, Leong KF, Barankin B. Lichen striatus with nail involvement in a 6-year-old boy. Case Rep Pediatr. 2020;2020:1494760. doi: 10.1155/2020/1494760.
8. Charifa A, Jamil RT, Ramphul K. Lichen striatus. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–2020 Nov 30. PMID: 29939607.
9. Karp DL, Cohen BA. Onychodystrophy in lichen striatus. Pediatr Dermatol. 1993;10(4):359-361. doi: 10.1111/j.1525-1470.1993.tb00399.x.
10. Jones J, Marquart JD, Logemann NF, DiBlasi DR. Lichen striatus-like eruption in an adult following hepatitis B vaccination: a case report and review of the literature. Dermatol Online J. 2018 Jul 15;24(7):13030/qt1hr764kv.
11. Fogagnolo L, Barreto JA, Soares CT, Marinho FC, Nassif PW. Lichen striatus on adult. An Bras Dermatol. 2011;86(1)142-145. doi: 10.1590/s0365-05962011000100022.
12. Amer A. Bilateral onychodystrophy in a boy with a history of isolated lichen striatus. Cutis. 2014;94(5):E16-19. PMID: 25474462.
13. Racette AJ, Adams AD, Kessler SE. Simultaneous lichen striatus in siblings along the same Blaschko line. Pediatr Dermatol. 2009;26(1):50-54. doi: 10.1111/j.1525-1470.2008.00821.x.
14. Zhang Y, McNutt NS. Lichen striatus. Histological, immunohistochemical, and ultrastructural study of 37 cases. J Cutan Pathol. 2001;28(2):65-71. doi: 10.1034/j.1600-0560.2001.280202.x.
15. Chong JH, Mermin D, Goussot JF, Taïeb A. Vitiligo co-existing with lichen striatus: more than a coincidence? J Eur Acad Dermatol Venereol. 2017;31(4):e200-e202. doi: 10.1111/jdv.13954.
16. Correia LD, Silva de Castro CC. Association between bilateral segmental vitiligo and lichen striatus: an expression of mosaicism? Int J Dermatol. 2018;57(8):992-993. doi: 10.1111/ijd.13964.
17. Gündüz Ö, Çakartaş R, Demirkan S, Atasoy P. Candidal vulvitis: a possible trigger for lichen striatus. Eur J Dermatol. 2018;28(4):521-523. doi: 10.1684/ejd.2018.3315.
18. Gupta A, Gautam RK, Bhardwaj M. Bilateral lichen striatus: A case report with review of literature. Indian Dermatol Online J. 2017;8(4):264-266. doi: 10.4103/idoj.IDOJ_304_16.
19. Gupta D, Mathes E. Lichen striatus. In: Post TW, ed. UpToDate. Waltham, MA. (Accessed on February 14, 2021)
20. Ishikawa M, Ohashi T, Yamamoto T. Lichen striatus following influenza infection. J Dermatol. 2014;41(12):1133-1134. doi: 10.1111/1346-8138.12684.
21. Karouni M, Kurban M, Abbas O. Lichen striatus following yellow fever vaccination in an adult woman. Clin Exp Dermatol. 2017;42(7):823-824. doi: 10.1111/ced.13167.
22. Lora V, Kanitakis J, Latini A, Cota C. Lichen striatus associated with etanercept treatment of rheumatoid arthritis. J Am Acad Dermatol. 2014;70(4):e90-e92. doi: 10.1016/j.jaad.2013.11.039.
23. Mask-Bull L, Vangipuram R, Carroll BJ, Tarbox MB. Lichen striatus after interferon therapy. JAAD Case Rep. 2015;1(5):254-256. doi: 10.1016/j.jdcr.2015.05.002.
24. Richarz NA, Fustà-Novell X, Fatsini-Blanch V, Fortuny C, González-Enseñat MA, Vicente A. Lichen striatus following scarlet fever in a 3-year-old female patient. Int J Dermatol. 2018;57(9):1118-1119. doi: 10.1111/ijd.13995.
25. Wollina U. Digital lichen striatus: Two case reports, one with onychodystrophy. Skin Appendage Disord. 2017;3(4):188-189. doi: 10.1159/000475554.
26. Unal E, Balta I, Bozkurt O. Lichen striatus: after a bite by bumblebee. 2015;34(2):171-172. doi: 10.3109/15569527.2014.910804.
27. Shepherd V, Lun K, Strutton G. Lichen striatus in an adult following trauma. Australas J Dermatol. 2005;46(1):25-28. doi: 10.1111/j.1440-0960.2005.00132.x.
28. Goyal S, Cohen BA. Lichen striatus. Arch Pediatr Adolesc Med. 2001;155(2):197-198. doi: 10.1001/archpedi.155.2.197.
29. Mu EW, Abuav R, Cohen BA. Facial lichen striatus in children: retracing the lines of Blaschko. Pediatr Dermatol. 2013;30(3):364-366. doi: 10.1111/j.1525-1470.2012.01844.x.
30. Valerio E, Giordano C, Mameli S, Poles A, Cutrone M. Facial lichen striatus. Arch Dis Child. 2016;101(12):1148. doi: 10.1136/archdischild-2016-310826.
31. Dickman JS, Frandsen MD, Racette AJ. Asymmetric bilateral lichen striatus: A rare presentation following multiple Blaschko's lines. Case Rep Dermatol Med. 2018;2018:6905175. doi: 10.1155/2018/6905175.
32. Sato H, Shirai A, Asahina A. Case of lichen striatus presenting with multiple lesions along Blaschko's lines. J Dermatol. 2012;39(9):802-804. doi: 10.1111/j.1346-8138.2011.01427.x.
33. Campanati A, Brandozzi G, Giangiacomi M, Simonetti O, Marconi B, Offidani AM. Lichen striatus in adults and pimecrolimus: open, off-label clinical study. Int J Dermatol. 2008;47(7):732-736. doi: 10.1111/j.1365-4632.2008.03654.x.
34. Iorizzo M, Rubin AI, Starace M. Nail lichen striatus: Is dermoscopy useful for the diagnosis? Pediatr Dermatol. 2019;36(6):859-863. doi: 10.1111/pde.13916.
35. Brys AK, Bellet JS. Pediatric dermatology photoquiz: Persistent lesion of the thumbnail of a 3-year-old boy. Lichen striatus. Pediatr Dermatol. 2016;33(1):95-6. doi: 10.1111/pde.12732.
36. Krishnegowda SY, Reddy SK, Vasudevan P. Lichen striatus with onychodystrophy in an infant. Indian Dermatol Online J. 2015;6(5):333-335. doi: 10.4103/2229-5178.164489.
37. Kim DW, Kwak HB, Yun SK, Kim HU, Park J. Dermoscopy of linear dermatosis along Blaschko's line in childhood: Lichen striatus versus inflammatory linear verrucous epidermal nevus. J Dermatol. 2017;44(12):e355-e356. doi: 10.1111/1346-8138.14035.
38. Dańczak-Pazdrowska A, Pawlaczyk-Gabriel K, Bowszyc-Dmochowska M, et al. Reverse Kobner response in lichen striatus: the first case described in the literature. Postepy Dermatol Alergol. 2018;35(4):434-435. doi: 10.5114/ada.2018.75840.


