Skin Disorders in Older Adults: Benign Growths and Neoplasms
Authors:
Noah S. Scheinfeld, MD, JD
Columbia University
Citation:
Scheinfeld NS. Skin disorders in older adults: benign growths and neoplasms. Consultant. 2011;51(9):650-656.
ABSTRACT
Benign cutaneous growths and neoplasms are more common in older adults than in younger persons. Seborrheic keratoses are the most frequently seen neoplasms in the elderly. Treatment is usually not necessary unless the lesions are irritated. A variety of benign lesions involve proliferation of melanocytes, including dysplastic nevi, compound nevi, and intradermal nevi. Melanocytic nevi do not require removal unless melanoma is suspected. Actinic keratoses are found on sun-exposed skin of elderly white persons, particularly those who tend to burn frequently and tan poorly. About 2% to 5% of these lesions evolve into squamous cell carcinoma. Treatment options include topical 5-fluorouracil, topical imiquimod, cryotherapy, curettage, photodynamic therapy, dermabrasion, chemical peels, laser treatment, and (rarely) surgery.
Keywords: seborrheic keratosis, stucco keratosis, benign melanocytic nevus, actinic keratosis, cutaneous horn, blue nevus, lentigo, porokeratosis
The skin of elderly persons possesses a greater number of benign growths and neoplasms than the skin of younger and middle-aged persons. In this article, I discuss seborrheic keratosis, stucco keratosis, benign melanocytic nevus, cutaneous horn, actinic keratosis, blue nevus, lentigo, and porokeratosis.
SEBORRHEIC KERATOSIS
Seborrheic keratoses are the most common neoplasms in elderly persons and affect up to 60% of this population. Risk factors for these lesions are thought to include genetic predisposition, age, and history of sun exposure.1,2
The hallmark feature of seborrheic keratoses is their pasted-on appearance; the lesions can often be peeled off with the fingers. Macular seborrheic keratoses are round or oval and flat (Figure 1). The surface of seborrheic keratoses may be flat, velvety, smooth, or verrucous (Figure 2). The lesions are usually brown or yellow-white (Figure 3); however, they may be red, gray, wax-colored, yellowish, black, or white.

Figure 1. A macular seborrheic keratosis can be seen on the side of this woman’s face.

Figure 2. This verrucous lesion is a seborrheic keratosis.

Figure 3. Seborrheic keratoses are typically brown or yellow-white.
Seborrheic keratoses start as small lesions but can grow to more than 1 cm or (rarely) larger. They can appear on any part of the body but are most commonly found on the torso. They are not usually accompanied by inflammation or erythema. However, irritation can induce swelling and sometimes bleeding, oozing, and crusting, as well as a darkening of the pigment as a result of inflammation. Seborrheic keratoses may resemble warts, actinic keratoses, melanoma, or inflammatory dermatosis that manifests with scaly or verrucous papules.
Seborrheic keratoses are less common in black persons than in whites. However, a variant of seborrheic keratosis—dermatosis papulosa nigra—sometimes develops in black persons and those of Asian and Hispanic descent. These lesions consist of numerous pedunculated growths that primarily affect the face, neck, and upper chest (Figure 4). They appear at an earlier age than seborrheic keratoses.

Figure 4. The lesions on this woman’s face are dermatosis papulosa nigra, a variant of seborrheic keratosis that sometimes develops in African Americans and persons of Asian and Hispanic descent.
Treatment is usually not necessary unless the lesions are irritated. Treatment options include cryotherapy with dry ice, liquid nitrogen,3 electrodesiccation with or without curettage, curettage alone, shave biopsy or excision with a scalpel or laser, and dermabrasion surgery. Biopsy is indicated if the diagnosis is ambiguous.
The sign of Leser-Trélat refers to the eruption of innumerable widespread seborrheic keratoses that is thought to indicate internal malignancy. The most commonly reported neoplasm is adenocarcinoma, especially of the GI tract. Seborrheic keratoses can also erupt after an exacerbation of inflammatory dermatitis, such as a flare of eczema or a severe sunburn.
STUCCO KERATOSIS
Stucco keratosis is considered a variant of seborrheic keratosis.4 The name probably derives from the resemblance of the lesions to old stucco on the sides of houses. Stucco keratosis is thought to result from thickening of the epidermis, in particular the stratum corneum, which histologically resembles a church spire.
The lesions are white or gray delled keratotic papules smaller than 5 mm (Figure 5); they are typically found on the legs of elderly men. When the lesions are removed, they leave a peripheral collarette of scale. Stucco keratoses are sometimes confused with actinic keratoses. Treatment options include liquid nitrogen therapy and electrodesiccation with curettage.

Figure 5. This white delled keratotic papule on an elderly man’s leg is stucco keratosis, which is considered a variant of seborrheic keratosis.
BENIGN MELANOCYTIC NEVUS
A variety of benign lesions in elderly patients involve proliferation of melanocytes.5,6 These lesions include dysplastic nevi, which histologically contain somewhat asymmetric nests of melanocytes (Figure 6); compound nevi, which histologically contain more symmetric nests of melanocytes in the dermis and epidermis (Figure 7); and intradermal nevi, which histologically contain nests of melanocytes in the dermis (Figure 8). Melanocytic nevi do not require removal unless a melanoma is suspected.

Figure 6. The dark brown lesion seen here is a dysplastic nevus.

Figure 7. A compound nevus is shown here.

Figure 8. This flesh-colored papule on a man’s nose is an intradermal nevus.
CUTANEOUS HORN
Cutaneous horn is a descriptive rather than diagnostic term that refers to horn projections of tissue (Figure 9) that are caused by a variety of neoplasms, including actinic keratosis, warts, Bowen disease, granular cell tumors, Paget disease, sebaceous neoplasms, basal and squamous cell carcinoma, and seborrheic keratosis.7 Rarely, molluscum contagiosum of the poxvirus group forms a cutaneous horn. The only other infectious cause is leishmaniasis. Cutaneous horns are removed by shave biopsy, and the tissue is sent for histologic examination.

Figure 9. This cutaneous horn had been present for several years before the patient sought medical attention.
ACTINIC KERATOSIS
Actinic (solar) keratoses are found on sun-exposed skin of elderly white persons—in particular redheaded or blond patients, who tend to burn frequently and tan poorly.8 Actinic keratoses are the most common sun-related growths in white persons. More than 60% of predisposed white persons older than 40 years have at least one actinic keratosis. About 2% to 5% of these lesions evolve into squamous cell carcinoma.
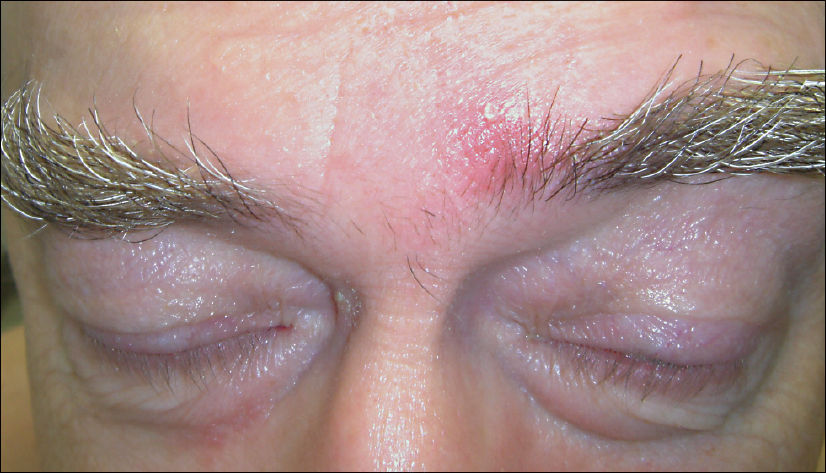
Most actinic keratoses consist of irregular white scaly papules with an erythematous base (Figure 10). Lesions with thickly keratotic surfaces are referred to as hypertrophic actinic keratoses (Figure 11), and they may be pigmented (Figure 12). They are usually 3 to 10 mm in diameter and enlarge gradually. Histologically, actinic keratoses demonstrate acanthosis, parakeratosis, and dyskeratoses with cellular atypia and keratinocytes with miotic figures that vary in size and shape.

Figure 10. The scaly, erythematous papule seen here is an actinic keratosis, which commonly occurs on the sun-exposed skin of elderly white persons.

Figure 11. This hypertrophic actinic keratosis has a thickly keratotic surface.

Figure 12. A pigmented actinic keratosis is shown here.
Often, the upper back of a patient with severely sun-damaged skin demonstrates patches of solar lentigines with distinct areas of scale. On palpation, the scaly areas demonstrate the slightly rough texture that characterizes actinic keratoses.
Actinic keratosis can flare and become more noticeable with immunosuppression, such as from acute sun exposure or chemotherapy (especially with systemic 5-fluorouracil).
The most common mimics of actinic keratosis are seborrheic keratosis, xerosis, seborrheic dermatitis, Bowen disease, superficial basal cell carcinoma, warts, porokeratosis, and squamous cell carcinoma. Less common varieties of actinic keratosis include hypertrophic actinic keratosis, pigmented actinic keratosis, and actinic keratosis related to cutaneous horn. Actinic keratosis on the lips is termed actinic cheilitis.
Treatment options include topical 5-fluorouracil, topical imiquimod, cryotherapy, curettage, photodynamic therapy, dermabrasion, chemical peels, carbon dioxide laser treatment, and (rarely) surgery.9,10 I prefer cryotherapy for discrete lesions and topical 5-fluorouracil cream for large areas where I suspect there are clinically unapparent lesions.
Actinic keratosis has a good prognosis. Treatment is determined by the extent of the patient’s lesions and his or her tolerance to pain and temporary inflammation. Such inflammation may be associated with cryotherapy, laser surgery, and topical 5-fluorouracil and imiquimod.
BLUE NEVUS
Blue nevi are a manifestation of dermal melanocytosis.11 They consist of blue, gray-blue (Figure 13), or brown-blue papules (Figure 14) that occur most commonly on the head and neck. The blue pigmentation is attributable to the depth of melanin in the dermis and the Tyndall effect (the preferential absorption of long light wavelengths by melanin and the scattering of shorter wavelengths, representing the blue end of the spectrum, by collagen bundles).

Figure 13. This gray-blue papule on a woman’s nose is a blue nevus, which is most common in persons of Asian descent.

Figure 14. Blue nevi occur most frequently on the head and neck, as in this patient.
Blue nevi are most frequently seen in Asian adults, in whom the prevalence is estimated to be 3% to 5%. They are found in 1% to 2% of white adults and rarely in blacks. They develop most commonly in younger persons but can appear in old age. Although blue nevi are benign, they are sometimes mistaken for melanomas, especially in elderly persons. Melanomas occasionally develop in association with blue nevi. This phenomenon is usually portended by rapid growth and, occasionally, ulceration of the nevus. In elderly persons, blue nevi that look irregular are best removed.
LENTIGO
Lentigines—small, well-demarcated tan or brown macules often encircled by sun-damaged skin—can also appear on normal skin (Figure 15). These macules, which become more numerous with advancing age, usually appear in groups (Figure 16).12 Typical histologic findings include thickening of the epidermis and increased pigmentation of the basal layer. Melanocytes may increase in number but they do not form nests. Lentigines may evolve gradually over time or they can erupt suddenly. The pigment ranges from tan to brown to black; it may be homogeneous or variegated.

Figure 15. This well-demarcated tan macule is a lentigo.

Figure 16. Lentigines usually appear in groups on a background of sun-damaged skin.
Patients sometimes request treatment for cosmetic reasons. Options include 20% to 50% trichloroacetic acid and cryotherapy (both of which may produce hypopigmentation that is usually transient) and topical products that contain hydroquinone or tretinoin.12
POROKERATOSIS
Porokeratosis is a clonal disorder of keratinization that features patches with raised red rims and atrophic centers.13 The histologic hallmark of porokeratosis is the cornoid lamella, the pathologic substrate of the ridgelike border. The 5 clinical variants of porokeratosis are classic porokeratosis of Mibelli (Figure 17); disseminated superficial actinic porokeratosis (DSAP) (Figure 18); porokeratosis palmaris et plantaris disseminata; linear porokeratosis; and punctate porokeratosis.

Figure 17. This patch with a raised red rim and atrophic center is classic porokeratosis of Mibelli.

Figure 18. Disseminated superficial actinic porokeratosis occurred in a patient with an history of excessive sun exposure.
DSAP, the most common type, is 3 times as likely to develop in women as in men. The typical patient is a woman in her third or fourth decade who has a history of excessive sun exposure. The condition manifests as innumerable small, indistinct light brown macules with threadlike red borders on the extensor surfaces of the arms and the legs. Malignant degeneration of DSAP into squamous cell carcinoma is seen primarily in elderly patients.
Treatment options include cryotherapy, laser ablation, photodynamic therapy, and topical 5-fluorouracil.
REFERENCES
- Pariser RJ. Benign neoplasms of the skin. Med Clin North Am. 1998;82:1285-1307, v-vi.
- Elgart GW. Seborrheic keratoses, solar lentigines, and lichenoid keratoses. Dermatoscopic features and correlation to histology and clinical signs. Dermatol Clin. 2001;19:347-357.
- Andrews MD. Cryosurgery for common skin conditions. Am Fam Physician. 2004;15:2365-2372.
- Shall L, Marks R. Stucco keratoses. A clinicopathological study. Acta Derm Venereol. 1991;71:258-261.
- Strungs I. Common and uncommon variants of melanocytic naevi. Pathology. 2004;36:396-403.
- Schaffer JV, Bolognia JL. The clinical spectrum of pigmented lesions. Clin Plast Surg. 2000;27:391-408, viii.
- Hoffman PC, Lenet MD, Sherman M. Cutaneous horns: review of literature and case report. J Foot Surg. 1988;27:130-133.
- Berman R, Bienstock L, Kuritzky L, et al; Primary Care Education Consortium; Texas Academy of Family Physicians. Actinic keratoses: sequelae and treatments. Recommendations from a consensus panel. J Fam Pract. 2006;55(suppl):1-8.
- Andrews MD. Cryosurgery for common skin conditions. Am Fam Physician. 2004;15:2365-2372.
- Gold MH, Nestor MS. Current treatment of actinic keratosis. J Drugs Dermatol. 2006;5(2 suppl):17-25.
- Gonzalez-Campora R, Galera-Davidson H, Vazquez-Ramirez FJ, Diaz-Cano S. Blue nevus: classical types and new related entities. A differential diagnostic review. Pathol Res Pract.1994;190:627-635.
- Ortonne JP, Pandya AG, Lui H, Hexsel D. Treatment of solar lentigines. J Am Acad Dermatol.2006;54(5 suppl 2):S262-S271.
- Sehgal VN, Jain S, Singh N. Porokeratosis. em>J Dermatol. 1996;23:517-525.