Enhance Your Dermatologic Prowess

Match the following characteristics with the clinical disorders pictured in the photographs of Cases 1 and 2. Then read the brief descriptions that follow to see how well you did.

Answers and Discussion on next page
DISCUSSION
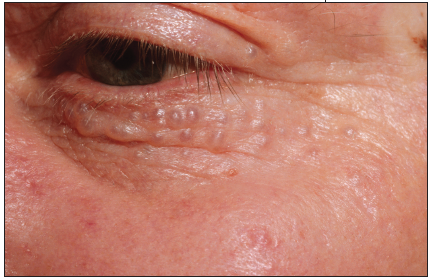
Both of the common disorders presented in Cases 1 and 2 typically have the face as the primary site of involvement, and both are benign tumors. Case 1 depicts hidrocystomas, while Case 2 demonstrates a classic example of syringomas.
Case 1 is a 52-year-old man whose skin lesions first developed 6 months before presentation. Since that time, the lesions have been slowly increasing in size and number. The globoid, 3- to 4-mm, fluid-filled, and slightly blue-hued translucent papules are asymptomatic.
 The hidrocystoma represents a cystic ectasia of sweat glands. There are two basic varieties: eccrine and apocrine.1 The former type is characterized by multiple, smaller (1- to 3-mm), distinctly blue-colored lesions, which may also involve the neck; the latter type typically presents with a single or just a few, larger (2- to 15-mm) lesions, most often surrounding the eyes. Apocrine hidrocystomas may also rarely be found in the anogenital region.
The hidrocystoma represents a cystic ectasia of sweat glands. There are two basic varieties: eccrine and apocrine.1 The former type is characterized by multiple, smaller (1- to 3-mm), distinctly blue-colored lesions, which may also involve the neck; the latter type typically presents with a single or just a few, larger (2- to 15-mm) lesions, most often surrounding the eyes. Apocrine hidrocystomas may also rarely be found in the anogenital region.
Hidrocystomas of both types occur randomly. They are encountered equally often in both men and women, and there is no known genetic predisposition.
Although these tumors have no long-term consequences, patients often desire removal for cosmetic reasons. Spontaneous resolution does not usually occur. Treatment requires punch, scissors, or elliptical excision with complete removal of the cyst wall. Alternatively, destruction can often be accomplished by application of 10% to 20% trichloroacetic acid or by electrodesiccation or laser ablation.2,3 Recurrence is infrequent. Cosmetically objectionable scarring may follow excessively vigorous attempts at destruction.
Case 2 is a 63-year-old woman whose skin lesions had been developing for many years before presentation. As in this patient, the typical onset of syringomas is at or near puberty, with the number of lesions increasing slowly but steadily thereafter. Syringomas are most often incidental, although some familial cases have been reported. However, neither a specific inheritance pattern nor a genetic defect has been identified. There is an increased prevalence in association with Down syndrome.4
 Syringomas usually occur on the upper cheeks and lower eyelids; uncommon sites of involvement include the axilla, chest, abdomen, penis, and vulva. Enzyme and cytokeratin immunohistochemical staining patterns, as well as ultrastructural findings, verify that these tumors arise from elements of the eccrine sweat gland duct. Syringomas are generally 3 mm or less in greatest dimension and are usually flat-topped to very slightly dome-shaped; color ranges from flesh-tone to yellowish.
Syringomas usually occur on the upper cheeks and lower eyelids; uncommon sites of involvement include the axilla, chest, abdomen, penis, and vulva. Enzyme and cytokeratin immunohistochemical staining patterns, as well as ultrastructural findings, verify that these tumors arise from elements of the eccrine sweat gland duct. Syringomas are generally 3 mm or less in greatest dimension and are usually flat-topped to very slightly dome-shaped; color ranges from flesh-tone to yellowish.
Treatment of syringomas is strictly for cosmetic reasons and is accomplished by some form of ablation. Various lasers, liquid nitrogen cryosurgery, electrodesiccation, and simple snip excision with pressure hemostasis have all been employed successfully.5,6 As is true with all hamartomas, the patient should be warned about recurrence and the potential for both scar formation and dyschromia following any type of destructive therapy.
The correct answers are as follows:

1. Bures FA, Kotynek J. Differentiating between apocrine and eccrine hidrocystoma. Cutis. 1982;29:616, 619-620.
2. Dailey RA, Saulny SM, Tower RN. Treatment of multiple apocrine hidrocystomas with trichloroacetic acid. Ophthal Plast Reconstr Surg. 2005;21:148-150.
3. del Pozo J, García-Silva J, Peña-Penabad C, Fonseca E. Multiple apocrine hidrocystomas: treatment with carbon dioxide laser vaporization. J Dermatolog Treat. 2001;12:97-100.
4. Schepis C, Siragusa M, Palazzo R, et al. Palpebral syringomas and Down’s syndrome. Dermatology. 1994;189:248-250.
5. Al Aradi IK. Periorbital syringoma: a pilot study of the efficacy of low-voltage electrocoagulation. Dermatol Surg. 2006;32:1244-1250.
6. Park HJ, Lee DY, Lee JH, et al. The treatment of syringomas by CO2 laser using a multiple-drilling method. Dermatol Surg. 2007;33:310-313.


