Six Common But Underrecognized Drug Interactions and Adverse Effects
Author:
Douglas Paauw, MD, MACP
Citation:
Paauw D. Six common but underrecognized drug interactions and adverse effects. Consultant. 2017;57(8):454-457.
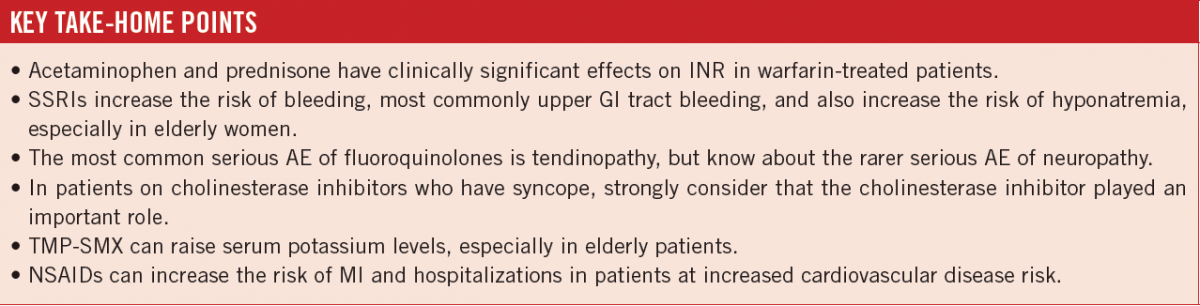
ABSTRACT: Medical problems and symptoms related to the use of medications are commonly encountered in primary care. In some cases, these are direct adverse effects (AEs) of the medications, while in other cases they are a result of drug interactions. It is difficult for health care providers to know and recognize the vast number of clinically significant drug interactions and AEs that occur with the use of medications. This article highlights the potential drug interactions and AEs of 6 commonly prescribed medications or classes of medications—warfarin, selective serotonin-reuptake inhibitors, fluoroquinolones, cholinesterase inhibitors, trimethoprim-sulfamethoxazole, and nonsteroidal anti-inflammatory drugs—and points out the clinical circumstances in which patients’ risk of experiencing these problems is greatest.
KEYWORDS: Warfarin, selective serotonin-reuptake inhibitors, fluoroquinolones, cholinesterase inhibitors, trimethoprim-sulfamethoxazole, nonsteroidal anti-inflammatory drugs, hyponatremia, syncope, hyperkalemia, prednisone, acetaminophen
Patients’ use of medications can cause a wide variety of signs, symptoms, and medical conditions, some of which are direct adverse effects (AEs) of a medication, while others are the result of drug-drug interactions. Because of the ubiquity and diversity of these signs and symptoms, recognizing their association with a medication or medications poses a diagnostic challenge to primary care providers.
This article reviews the potential drug interactions and AEs of 6 commonly prescribed medications or classes of medications—warfarin, selective serotonin-reuptake inhibitors (SSRIs), fluoroquinolones, cholinesterase inhibitors, trimethoprim-sulfamethoxazole (TMP-SMX), and nonsteroidal anti-inflammatory drugs (NSAIDs)—and discusses the clinical circumstances in which patients’ risk of experiencing these problems is greatest, with the goal of avoiding the potentially serious threats to patients’ health.
Warfarin Interactions
The most common cause for emergency department (ED) visits for adverse drug events in the United States is bleeding associated with anticoagulant use, with the majority of cases related to the use of warfarin.1 Nearly half of the patients seen in US EDs for warfarin-related bleeding were admitted to the hospital.1 Several warfarin drug interactions are important to highlight because they occur so frequently and involve commonly used medications.
TMP-SMX interactions with warfarin are the most common serious drug interactions encountered with warfarin. In a study of patients receiving antibiotics while taking warfarin, the average increase in international normalized ratio (INR) was 1.76 for patients taking TMP-SMX.2 Avoiding prescribing TMP-SMX to patients on warfarin is the safest approach. If no alternative antibiotic is available, then dose reduction of the warfarin by 10% to 20% can help maintain the INR in the therapeutic range.3 The medications aside from TMP-SMX with the most consistent and severe interactions with warfarin that raise INR are erythromycin, amiodarone, fluconazole, ketoconazole, itraconazole, and metronidazole.
Acetaminophen can have a significant interaction with warfarin. Hylek and colleagues conducted a case-control study and found that patients on warfarin who ingested 9100 mg or more of acetaminophen per week for more than 1 week had a 10-fold increased risk of having an INR greater than 6.4 Zhang and colleagues studied the effect of acetaminophen on patients taking warfarin, with 45 patients on stable warfarin therapy randomly assigned to either acetaminophen 2 or 3 g daily or placebo.5 The mean increase in INR was 0.70 for patients receiving 2 g acetaminophen a day and 0.67 for those receiving 3 g a day. The interaction with warfarin is a particular concern for patients taking regular daily acetaminophen, but it is unlikely to be a significant problem when patients take an occasional dose of acetaminophen for transient symptoms.
Another interaction with warfarin that is underrecognized is with prednisone. In a retrospective study done at an anticoagulation clinic, patients receiving warfarin and prednisone showed a significant increase in INR.6 The study excluded all patients on warfarin and prednisone who were also receiving any additional drugs with known interactions with warfarin. The mean difference in INR before and after being started on the corticosteroid was 1.24 (95% CI, 0.86-1.62; P < .001). More than 62% of the patients had an INR out of the target zone, with the mean time to maximum INR being 6.7 days. The most important point about this interaction is to recognize it in the first place. Because most patients treated with prednisone take it for a short time, the effect will be transient. In many cases, dose adjustment of warfarin will not be necessary. Dowd and colleagues found that warfarin dose reduction led to no significant difference in regards to excessive anticoagulation in patients receiving prednisone.7 A higher percentage of patients who had a warfarin dose reduction had a subtherapeutic INR compared with patients who did not receive a dose reduction (40% vs 5.9%, P = .02).
Selective Serotonin-Reuptake Inhibitors
The most common AEs related to the use of SSRIs are sexual AEs, occurring in 17% of patients.8 The 2 most dangerous AEs associated with the use of SSRIs are increased risk of upper gastrointestinal (GI) tract bleeding and hyponatremia. Patients who are taking an SSRI have a 3- to 4-fold increased risk of having an upper GI bleed (UGIB).9,10 If a patient is also taking an NSAID, the relative risk of UGIB is greater than 6, according to the results of a study by Loke and colleagues.11 They found that the number needed to harm (NNH) in association with UGIB for patients on an SSRI was 411 patients per year. If patients also were taking an NSAID along with an SSRI, the NNH was 106 per year. If patients had a history of UGIB and had been on antiulcer medications in the past, the NNH was 70 per year. The use of SSRIs is associated with a higher risk of non–ulcer-related bleeding.
SSRIs have been recognized as a cause of hyponatremia for the past 2 decades. All SSRIs have been implicated, along with serotonin-norepinephrine reuptake inhibitors. It is difficult to accurately calculate the risk of hyponatremia associated with SSRI use. The only published prospective study looked at 75 older patients (aged 63-90 years) treated with paroxetine over a 12-week period.12 Hyponatremia developed in 12% of the patients, occurring at a mean time of 9 days. Certain risk factors have been associated with an increased risk of the development of SSRI-associated hyponatremia, including advanced age, low body mass, female sex, and concurrent diuretic use.13 Patients who are taking diuretics, particularly hydrochlorothiazide, are at especially higher risk for more-severe hyponatremia.
Fluoroquinolones
In July 2016, the Food and Drug Administration (FDA) changed the labeling of fluoroquinolones to advise not using these drugs for cystitis, sinusitis, and acute exacerbations of chronic bronchitis. The reason for this change was a concern over disabling AEs related to fluoroquinolones.
In 2013, the FDA sent a letter to all US prescribers warning about fluoroquinolone-induced neuropathy, which had been first described in the 1990s.14 The onset of neuropathy is usually within the first 72 hours of starting the medication, and it can be permanent.
In 2008, the FDA sent a warning letter that a black box warning had been added to the label of fluoroquinolones regarding the associated risk for tendonitis and tendon rupture. One study found that those at highest risk for the development of Achilles tendinopathy while on fluoroquinolones are patients older than 60 years (odds ratio [OR], 8.3 in patients > 60 vs 1.6 in patients < 60) and patients on corticosteroids (OR, 9.1 vs 3.2 in patients not on steroids).15
Several recent studies have suggested a new and very dangerous possible AE of fluoroquinolones. Lee and colleagues conducted a case-control study of patients admitted with aortic aneurysm or aortic dissection and fluoroquinolone exposure.16 Current use of fluoroquinolones was found to be associated with increased risk for aortic aneurysm or dissection with a rate ratio of 2.4, and past use was associated with a rate ratio of 1.48. In another study looking at collagen-related AEs in fluoroquinolone users, Daneman and colleagues found a hazard ratio (HR) of 3.13 for tendon rupture and a HR of 2.72 for aortic aneurysms.17
NEXT: Cholinesterase Inhibitors, Trimethoprim-Sulfamethoxazole, and NSAIDS
Cholinesterase Inhibitors
Cholinesterase inhibitors such as donepezil are commonly used as treatment for patients with dementia. The drug class has a high incidence of AEs, which may outweigh the modest benefits in a significant number of patients who are prescribed the drug. Common AEs related to the use of cholinesterase inhibitors include GI tract symptoms (nausea, vomiting, diarrhea) and weight loss.18
Urinary incontinence can occur with cholinesterase inhibitors, and the correlation with starting the drug is often overlooked.19,20 It is easy to assume that a patient’s urinary incontinence is a result of the progression of dementia and to attempt to treat the incontinence with an anticholinergic drug. However, anticholinergic drug therapy for incontinence is likely to worsen cognitive impairment, which was the reason for the cholinesterase regimen in the first place.
Syncope is a very serious AE that has been linked to cholinesterase inhibitors. Cholinesterase inhibitors are associated with development of bradycardia. Gill and colleagues looked at the association of cholinesterase inhibitor use with syncope, permanent pacemaker placement, and hip fractures in a population-based cohort study.21 They found an HR of 1.76 for syncope, an HR of 1.69 for bradycardia, an HR of 1.49 for permanent pacemaker placement, and an HR of 1.18 for hip fracture.
Given the modest benefit of cholinesterase inhibitors and the high morbidity and mortality associated with falls in patients with dementia, cholinesterase inhibitors should be discontinued in such patients who have a syncopal event. It would also be reasonable to discontinue a cholinesterase inhibitor before considering a permanent pacemaker, since cholinesterase inhibitors have been associated with reversible second-degree atrioventricular block and with bradycardia.22
Trimethoprim-Sulfamethoxazole
Hyperkalemia is an often-overlooked AE associated with the use of TMP-SMX. It is much more likely to occur in patients with kidney disease and in the elderly population. Hyperkalemia is also more likely to occur in patients who are taking angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs).23 The use of TMP-SMX has been linked to an increased risk of sudden cardiac death in patients who are receiving ACEIs or ARBs, possibly due to hyperkalemia.24
Witt and colleagues studied the effect of standard-dose TMP-SMX on serum potassium in elderly men at a Department of Veterans Affairs medical center.25 All patients who were on medications that could increase potassium or who had chronic renal insufficiency were excluded from the study. The authors compared the potassium levels of patients who received TMP-SMX with those who received other antibiotics. The serum potassium concentration in the group receiving TMP-SMX was 4.22 ± 0.40 mmol/L and increased by 0.31 ± 0.38 mmol/L at the end of therapy. There was no change in the serum potassium level of patients who received other antibiotics.
Trimethoprim has the same effect on the distal nephron as amiloride, reducing tubular potassium excretion.26 Trimethoprim can also raise serum creatinine levels without causing kidney disease. Trimethoprim causes an age-independent reversible inhibition of the tubular secretion of creatinine.27 No kidney damage occurs, and the elevation in creatinine resolves within a week of stopping the medication. There is no change in the glomerular filtration rate despite the increase in creatinine that can occur with trimethoprim.
Nonsteroidal Anti-inflammatory Drugs
NSAIDs are frequently used and are widely available over the counter. They are much more associated with toxicity when used by elderly patients. The complications related to the GI tract and renal toxicity of NSAIDs are widely known, and the scope of the problem is enormous. It is estimated that more than 100,000 hospitalizations occur in the United States each year related to NSAID-induced GI tract bleeding, at an annual cost of more than $2 billion.28 NSAID-related renal toxicity is much more likely to occur in patients who are elderly, who have preexisting kidney disease, and/or who are taking other potentially nephrotoxic drugs.
Very important drug interactions of NSAIDs are with ACEIs, ARBs, and diuretics. The combination of ACEIs or ARBs with diuretics and NSAIDs increases the risk of acute kidney injury.29 The use of NSAIDs may make the antihypertensive effects of ACEIs and ARBs less effective and lead to intensification of blood pressure regimens.30
NSAID use increases the risk of myocardial infarction (MI) in patients with a history of coronary artery disease and also increases the risk of hospitalization for heart failure. A nationwide cohort study in Denmark of patients taking NSAIDs after a first MI found a significant association between NSAID use and recurrent MI after as little as 1 week of treatment.31 A large meta-analysis of 280 trials of NSAIDs (including traditional NSAIDS and selective cyclooxygenase 2 [COX-2] inhibitors) vs placebo or other NSAIDs found that major vascular events were increased by approximately one-third by selective COX-2 inhibitors or diclofenac; ibuprofen also significantly increased major coronary events.32
In July 2015, the FDA strengthened the warning on NSAIDs about the link to cardiovascular disease in patients with a history of or at high risk for coronary artery disease.33
Douglas Paauw, MD, MACP, is a professor of medicine and the Rathmann Family Foundation Endowed Chair in Patient-Centered Clinical Education at the University of Washington School of Medicine in Seattle, Washington.
REFERENCES:
- Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US emergency department visits for outpatient adverse drug events, 2013-2014. JAMA. 2016;316(20):2115-2125.
- Glasheen JJ, Fugit RV, Prochazka AV. The risk of overanticoagulation with antibiotic use in outpatients on stable warfarin regimens. J Gen Intern Med. 2005;20(7):653-656.
- Ahmed A, Stephens JC, Kaus CA, Fay WP. Impact of preemptive warfarin dose reduction on anticoagulation after initiation of trimethoprim-sulfamethoxazole or levofloxacin. J Thromb Thrombolysis. 2008;26(1):44-48.
- Hylek EM, Heiman H, Skates SJ, Sheehan MA, Singer DE. Acetaminophen and other risk factors for excessive warfarin anticoagulation. JAMA. 1998;279(9):657-662.
- Zhang Q, Bal-dit-Sollier C, Droeut L, et al. Interaction between acetaminophen and warfarin in adults receiving long-term oral anticoagulants: a randomized controlled trial. Eur J Clin Pharmacol. 2011;67(3):309-314.
- Hazelwood KA, Fugate SE, Harrison DL. Effect of oral corticosteroids on chronic warfarin therapy. Ann Pharmacother. 2006;40(12):2101-2106.
- Dowd MB, Vavra KA, Witt DM, Delate T, Martinez K. Empiric warfarin dose adjustment with prednisone therapy: a randomized, controlled trial. J Thromb Thrombolysis. 2011;31(4):472-477.
- Hu XH, Bull SA, Hunkeler EM, et al. Incidence and duration of side effects and those rated as bothersome with selective serotonin reuptake inhibitor treatment for depression: patient report versus physician estimate. J Clin Psychiatry. 2004;65(7):959-965.
- Dalton SO, Johansen C, Mellemkjær L, Sørensen HT, Nørgård B, Olsen JH. Use of selective serotonin reuptake inhibitors and risk of upper gastrointestinal tract bleeding a population-based cohort study. Arch Intern Med. 2003;163(1):59-64.
- de Abajo FJ, Rodríquez LAG, Montero D. Association between selective serotonin reuptake inhibitors and upper gastrointestinal bleeding: population based case-control study. BMJ. 1999;319(7217):1106-1109.
- Loke YK, Tivedi AN, Singh S. Meta-analysis: gastrointestinal bleeding due to interaction between selective serotonin uptake inhibitors and non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther. 2008;27(1):31-40.
- Fabian TJ, Amico JA, Kroboth PD, et al. Paroxetine-Induced hyponatremia in older adults: a 12-week prospective study. Arch Intern Med. 2004;164(3):327-332.
- Jacob S, Spinier SA. Hyponatremia associated with selective serotonin-reuptake inhibitors in older adults. Ann Pharmacother. 2006;40(9):1618-1622.
- Hedenmalm K, Spigset O. Peripheral sensory disturbances related to treatment with fluoroquinolones. J Antimicrob Chemother. 1996;37(4):831-837.
- Wise BL, Peloquin C, Choi H, Lane NE, Zhang Y. Impact of age, sex, obesity, and steroid use on quinolone-associated tendon disorders. Am J Med. 2012;125(12):1228.e23-1228.e28.
- Lee C-C, Lee M-t, Chen Y-S, et al. Risk of aortic dissection and aortic aneurysm in patients taking oral fluoroquinolone. JAMA Intern Med. 2015;175(11):1839-1847.
- Daneman N, Lu H, Redelmeier DA. Fluoroquinolones and collagen associated severe adverse events: a longitudinal cohort study. BMJ Open. 2015;5(11):e010077.
- Sheffrin M, Miao Y, Boscardin WJ, Steinman MA. Weight loss associated with cholinesterase inhibitors in individuals with dementia in a national healthcare system. J Am Geriatr Soc. 2015;63(8):1512-1518.
- Starr JM. Cholinesterase inhibitor treatment and urinary incontinence in Alzheimer’s disease. J Am Geriatr Soc. 2007;55(5):800-801.
- Hashimoto M, Imamura T, Tanimukai S, et al. Urinary incontinence: an unrecognised adverse effect with donepezil. Lancet. 2000;356(9229):568.
- Gill SS, Anderson GM, Fischer HD, et al. Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors a population-based cohort study. Arch Intern Med. 2009;169(9):867-873.
- Hundae A, Afzal A, Assar MD, Schussler JM. Syncope secondary to second-degree atrioventricular block with donepezil use. Proc (Bayl Univ Med Cent). 2014;27(4):325-326.
- Antoniou T, Gomes T, Juurlink DN, Loutfy MR, Glazier RH, Mamdani MM. Trimethoprim-sulfamethoxazole-induced hyperkalemia in patients receiving inhibitors of the renin-angiotensin system: a population-based study. Arch Intern Med. 2010;170(12):1045-1049.
- Scheper H, Lijfering WM. Link between co-trimoxazole and sudden death in patients receiving inhibitors of renin-angiotensin system could be due to confounding. BMJ. 2014;349:g6899.
- Witt JM, Koo JM, Danielson BD. Effect of standard-dose trimethoprim/sulfamethoxazole on the serum potassium concentration in elderly men. Ann Pharmacother. 1996;30(4):347-350.
- Velázquez H, Perazella MA, Wright FS, Ellison DH. Renal mechanism of trimethoprim-induced hyperkalemia. Ann Intern Med. 1993;119(4):296-301.
- Kastrup J, Petersen P, Bartram R, Hansen JM. The effect of trimethoprim on serum creatinine. Br J Urol. 1985;57(3):265-268.
- Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999;340(24):1888-1899
- Lapi F, Azoulay F, Yin H, Nessim SJ, Suissa S. Concurrent use of diuretics, angiotensin converting enzyme inhibitors, and angiotensin receptor blockers with non-steroidal anti-inflammatory drugs and risk of acute kidney injury: nested case-control study. BMJ. 2013;346:e8525.
- Fournier J-P, Sommet A, Bourrel R, et al. Non-steroidal anti-inflammatory drugs (NSAIDs) and hypertension treatment intensification: a population-based cohort study. Eur J Clin Pharmacol. 2012;68(11):1533-1140.
- Schjerning Olsen A-M, Fosbøl EL, Lindhardsen J, et al. Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study. Circulation. 2011;123(20):2226-2235.
- Coxib and traditional NSAID Trialists’ (CNT) Collaboration. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomized trials. Lancet. 2013;382(9894):769-779.
- FDA strengthens warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) can cause heart attacks or strokes. US Food and Drug Administration. https://www.fda.gov/downloads/Drugs/DrugSafety/UCM453941.pdf. Published July 9, 2015. Accessed July 7, 2017.


