Peer Reviewed
Kawasaki Disease
AUTHORS:
Claire Harrington, BS, and Robert Escalera, MD
CITATION:
Harrington C, Escalera R. Kawasaki disease. Consultant for Pediatricians. 2016;15(12):618-620.
A 6-month-old boy presented to the emergency department (ED) with a history of 2 days of vomiting, fever, and abdominal pain. He was followed overnight and discharged after abdominal ultrasonography did not reveal appendicitis or intussusception. The next day, his primary care provider treated him with amoxicillin due to a suspicion of an early otitis media.
The following day, the infant was assessed in the ED for continued fever of 4 days duration, vomiting, refusal to eat, poor urine output, and lethargy. There was an erythematous, maculopapular rash on all extremities, and bright erythema of the oral mucosa. His sclera were injected, but there was no discharge from his eyes. His hands and feet were edematous.
An unspun microscopic urinalysis (UA) showed 25 to 50 white blood cells/hpf and 10 to 25 red blood cells/hpf. In addition, laboratory test results showed a low albumin of 2.5 g/dL (reference range, 3.5-5.5 g/dL) and an elevated alanine aminotransferase (ALT) of 270 U/L (reference range, 8-20 U/L). The infant was admitted and treated with ceftriaxone for possible urinary tract infection.
Further laboratory test results revealed an elevated C-reactive protein (CRP) of 8.7 mg/dL (reference range, 0-1.0 mg/dL), a negative rapid viral polymerase chain reaction (PCR) nasal swab for multiple respiratory viruses (Table 1), and a negative rapid gastrointestinal PCR (Table 2) for multiple stool pathogens. The next day, the CRP doubled to 16.6 mg/dL and the fever persisted. The combination of 5 days of fever, supportive clinical findings, and absence of an infectious etiology via rapid testing led to the diagnosis of Kawasaki disease (KD).

An echocardiogram was performed and revealed a prominent left coronary artery that measured within normal limits and a right coronary artery that measured at the upper limits of normal size. The infant was treated with 3 daily doses of pulse-dose methylprednisolone (30 mg/kg), and a single 2 g/kg infusion of intravenous immunoglobulin (IVIG).1 The fever resolved within 24 hours of IVIG treatment, and the conjunctivitis and oral mucosa cleared by the third day. After the fourth day of hospitalization, the CRP normalized, and the patient was started on low-dose aspirin (40.5 mg/day). The infant was placed on a proton pump inhibitor to minimize gastrointestinal irritation resulting from treatment with the corticosteroid and aspirin. The platelets reached a peak of 835 × 103/µL (reference range, 200-450 ×103/µL) on day 14 and stayed elevated for about 1 month.
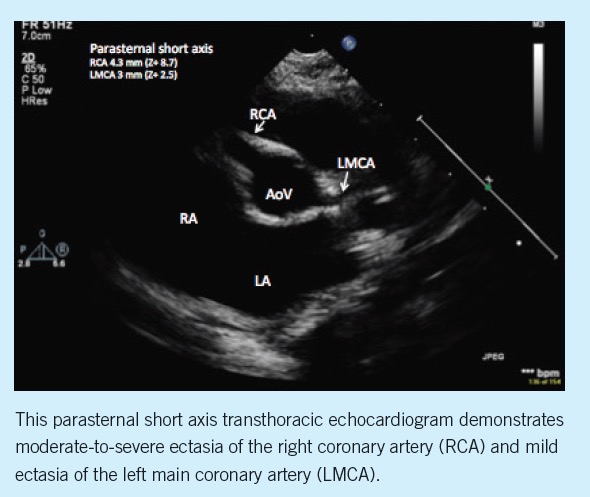
A follow-up cardiology evaluation was performed 2 weeks after hospital discharge. At this visit, an echocardiogram was performed and revealed diffuse right coronary artery ectasia, measuring 4.3 mm (Z-score +8.7). Additionally, there was mild ectasia of the left main coronary artery (3 mm, Z-score +2.5) and left anterior descending coronary artery (2.2 mm, Z-score +2.5) (Figure). Cardiac function was normal and there was a trivial pericardial effusion.


DISCUSSION
KD is an acute vasculitis of small- and medium-sized vessels and mostly affects children who are younger than 5 years. The classic diagnostic criteria for KD are fever for at least 5 days, bilateral nonpurulent conjunctival injection, changes in lips and oral cavities, polymorphous rash, changes in extremities, and cervical lymphadenopathy. This case met the requirements for typical KD, since the child met 4 out of the 5 criteria. Cervical lymphadenopathy was not present.
The peak incidence of KD is 6 to 23 months of age,2 but the disease may also affect children younger than 6 months and older than 8 years of age.3 Outside of this age range the presentation of KD might be atypical, with signs and symptoms becoming more variable and less likely to meet full criteria.3,4
Infants younger than 6 months of age are more likely to have an incomplete presentation.2 The guidelines of the American Heart Association for incomplete KD are 5 or more days of fever and fewer than 4 of the classic criteria.1 Children with incomplete KD also might have echocardiographic evidence of coronary artery aneurysms and should be treated even if they do not fit the full criteria. Incomplete KD should be considered and the child treated for KD if the CRP is ≥ to 3 mg/dL and 3 or more of the following laboratory criteria are present: albumin < 3.0 g/dL, anemia for age, elevation of ALT, platelets after day 7 ≥ 450 × 103 /µL, white blood cell (WBC) count ≥ 15 × 103 /µL, and/or urinalysis ≥ 10 WBC/hpf (in the absence of a positive culture).5
The mortality rate in KD is about 1% and is primarily a result of coronary artery involvement. Children younger than 6 months have the highest risk of coronary involvement.2,3,6,7 Atypical presentation of KD, especially in children outside the usual age range, might result in a delay in diagnosis. There is suspicion that coronary artery involvement might occur more frequently due to this delay in diagnosis.3 There also may be some physiologic differences in the children in the extremes of the pediatric age range that make them more susceptible to coronary artery involvement.3
The KD guidelines suggest treatment of KD and atypical KD by 10 days of symptoms to lower the risk of coronary artery involvement and to minimize mortality. The need for and dosage (high, medium, or low) of aspirin is controversial. Treatment with aspirin is thought to inhibit the inflammatory state of the coronary vessel intima and prevent thrombosis related to the subsequent elevation of platelets.1
An interesting feature to this case is that it introduces the use of the newer rapid antigen testing that allows the practitioner a chance to rule out other common viral pathogens that can sometimes cloud the path to an earlier diagnosis of KD. Prior to these rapid antigen tests, the treating practitioner needed to consider the likelihood of a viral pathogen such as adenovirus or parainfluenza mimicking the signs and symptoms of KD and thereby prolonging the phase of diagnostic uncertainty for days in cases of atypical KD, while the serology testing was being completed. The rapid antigen testing can be done in a matter of hours and provides the clinician with more information to alleviate the tension of giving IVIG before the 10-day window. No studies to date have examined the impact of these powerful new tools now available from laboratories and their impact on improvement in diagnostic accuracy. Although these new rapid tests are sensitive, they are not infallible and should not dissuade the experienced clinician from IVIG treatment if they are confident in their clinical diagnosis of KD.
Claire Harrington, BS, is a second-year medical student at University of Virginia Medical School in Charlottesville, Virginia.
Robert Escalera, MD, is a cardiologist at Children’s Hospital of The King’s Daughters in Norfolk, Virginia.
REFERENCES
1. Saguil A, Fargo M, Grogan S. Diagnosis and management of Kawasaki disease. Am Fam Physician. 2015;91(6):365-372.
2. Hangai M, Kubota Y, Kagawa J, et al. Neonatal Kawasaki disease: case report and data from nationwide survey in Japan. Eur J Pediatr. 2014;173(11):1533-1536.
3. Pannaraj PS, Turner CL, Bastian JF, Burns JC. Failure to diagnose Kawasaki disease at the extremes of the pediatric age range. Pediat Infect Dis J. 2004;23(8):789-791.
4. Stockheim JA, Innocentini N, Shulman ST. Kawasaki disease in older children and adolescents. J Pediatr. 2000;137(2):250-252.
5. Tacke CE, Breunis WB, Pereira RR, Breur JM, Kuipers IM, Kuijpers T. Five years of Kawasaki disease in the Netherlands: a national surveillance study. Pediatr Infect Dis J. 2014;33(8):793-797.
6. Chang FY, Hwang B, Chen S, Lee P, Meng C, Lu J. Characteristics of Kawasaki disease in infants younger than six months of age. The Pediatr Infect Dis J. 2006;25(3):241-244.
7. Hinze CH, Graham TB, Sutherell JS. Kawasaki disease without fever. The Pediatr Infect Dis J. 2009;28(10):927-928.


